
September 1, 2024
Urine Incontinence A Summary
6 Means To Treat Bladder Leakage This mechanical stress, combined with hormone influences, can weaken the pelvic flooring muscle mass, compromising their capability to keep urinary system continence. Consequently, several pregnant women experience symptoms of urinary system incontinence, such as anxiety urinary incontinence (SUI) or advise incontinence, particularly in the later phases of maternity. Women urinary system health is an intricate interaction of numerous aspects, with hormonal balance playing a crucial function.Treatment
What hormonal agent quits pee?
earn less pee during the night. Takeaway: If progesterone levels are rising during and after your cycle, and progesterone triggers your bladder to get a lot more frequently, it might trigger urinary incontinence. Menstruation adjustments. There are many factors your monthly duration can change, but hormonal discrepancy typically plays a role.Hair issues.

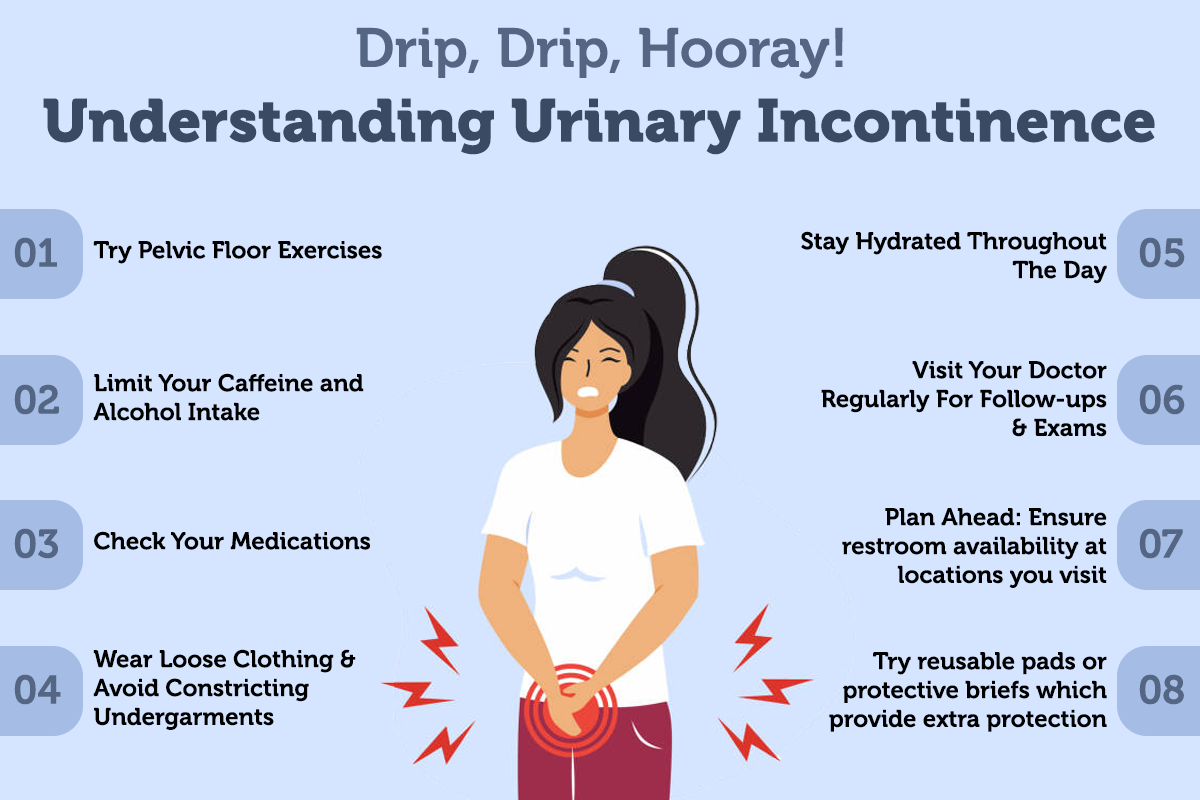
Pelvic Flooring Muscle Mass Exercises
Hormonal agent treatment (estrogen) in postmenopausal females minimizes urinary system regularity and dysuria and blood flow of bladder cells boosts and causes https://pain-relief.s3.us-east.cloud-object-storage.appdomain.cloud/Therapies/treatment/radiation.html raise the stamina of muscular tissues around the urethra [44] Steroid hormones in addition to ecological impacts in the urinary system system have a central role in the neural control of urination process. Nevertheless, the precise device of this action is unknown, yet the presence of both types of estrogen receptors in the brain cortex, limbic system, the hippocampus and the brain has actually been verified [36] If guided to pursue surgical treatment by your physician, timely action is suggested, as waiting might lower the efficiency of medical treatment. The point of views shared in client reviews are by people only; they are not certified medical professionals. These point of views should not be relied upon as, or instead of, the clinical recommendations of a certified physician, etc. Urinary system urinary incontinence is a common problem influencing several people, particularly postmenopausal females. Urethral incompetence usually leads to recurring urinary incontinence, usually at remainder. Hormonal agent treatment (estrogen) in postmenopausal females reduces urinary regularity which brings about raise in the stamina of muscles around the bladder. Althoughbasic scientific research around is restricted, a recent placebo-controlled, randomizedclinical test of estrogen alone sheds light on this issue. Urethral closureis depending on the incorporated action of the suburethral genital wall, thepubourethral tendons, the pubococcygeus muscle mass, and the paraurethral connectivetissues. As you age, the muscle mass that sustain your pelvic body organs can deteriorate. This suggests that your bladder and urethra have less support-- commonly leading to urine leak. It likewise helps keep your bladder and urethra healthy and balanced and working effectively. They might no more be able to regulate your bladder as they did previously. As your estrogen levels continue to go down throughout and after menopause, your UI signs might worsen. Estrogens, normally in the kind of diethylstilbestrol, are carried out to spayed women.- This decreases the elasticity and toughness of the vaginal canal and bordering muscles, minimizing muscle support for the bladder and related structures, such as the urethra.
- In those instances, your incontinence also normally stops once the condition is treated.
- In patients with mental deterioration, urinary incontinence and urinary tract disorder might be because of certain participation of the locations of the cortex involved in bladder control.
- Pelvic floor workouts (Kegels) can enhance muscles and reduce symptoms.
Social Links